|
Pain-free Fibromyalgia Classes in Guisborough at Physioplus+ https://www.physioplusguisborough.co.uk/articles/pain-free-fibromyalgia-classes-in-guisborough
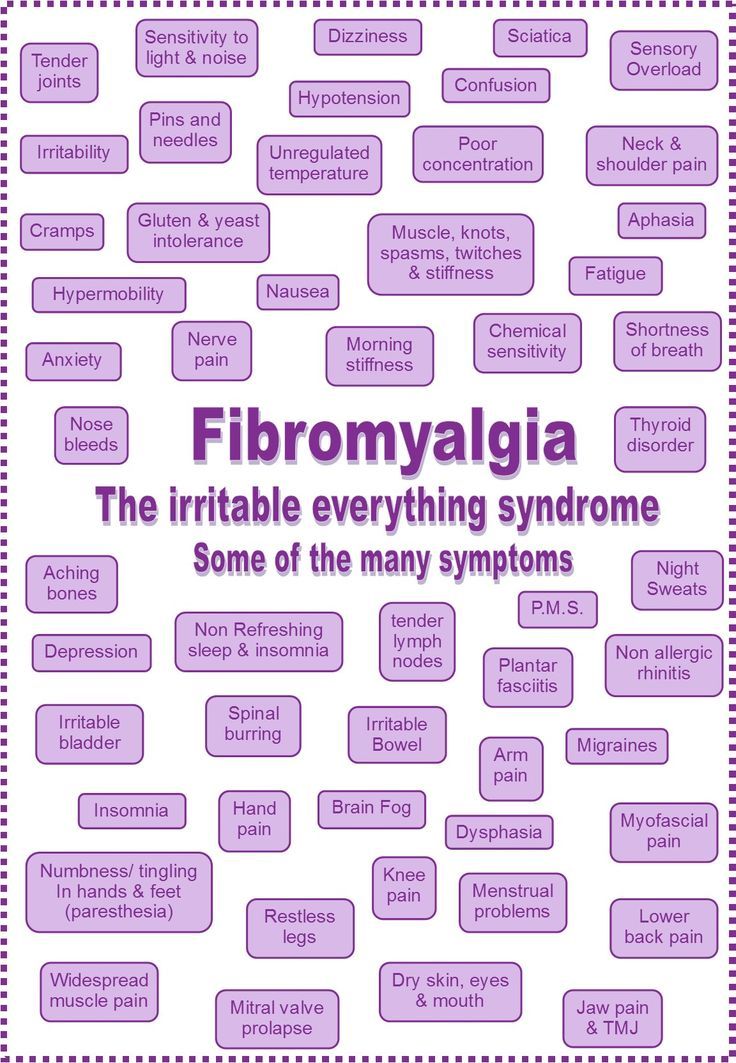
Fibromyalgia: Cracking the Case Researchers are just beginning to understand the biological underpinnings of a long-misunderstood condition. Fibromyalgia. Many patients with this perplexing diagnosis have seen doctor after doctor in search of an explanation for the widespread pain, fatigue, and disordered sleep that has disrupted their lives - sometimes severely. Depression, anxiety, and “brain fog” also commonly affect people with Fibromyalgia. Despite decades of research, seemingly everything about Fibromyalgia remains mysterious. But, encouragingly, researchers are finally making progress toward understanding this long-unexplained syndrome. Those who study Fibromyalgia hope this will legitimize a condition that physicians have long doubted, and bring much-needed relief to patients. A difficult diagnosis Not everyone with all-over pain receives the diagnosis of Fibromyalgia. The label usually comes from a Rheumatologist - a doctor who specializes in musculoskeletal and autoimmune disorders - only after other ailments are ruled out. But other chronic pain diagnoses, including temporomandibular joint disorder (TMJD), chronic pelvic pain conditions such as interstitial cystitis (IC), and irritable bowel syndrome (IBS) often mimic the symptoms of Fibromyalgia, also often with no discernible physical cause. The diagnosis that a patient receives might depend on the specialist they see, experts say. Roland Staud, University of Florida, Gainesville, US, likens the current understanding of fibromyalgia to the traditional Indian story of seven blind mice trying to determine the identity of an elephant. One blind mouse feels a leg and calls it a pillar; another grabs ahold of the tail and reports finding a rope. Not until all the parts are considered as a whole does a complete picture of the beast emerge. Likewise, Rheumatologists with patients complaining of muscle aches may diagnose Fibromyalgia, whereas a gastroenterologist proclaims IBS the cause of pain, but apart from complaints of regional pain in IBS, the overall symptoms of these two conditions look remarkably similar. Patients with low back pain, osteoarthritis, and other common chronic pain conditions can also develop this characteristic set of symptoms. Today, researchers are sketching out a picture of Fibromyalgia as a pain disorder that can be triggered by any number of individual maladies, each one heightening future risk for developing this enigmatic condition. Brain pain? Researchers and doctors have traditionally classified different types of pain into several categories. Nociceptive pain is the acute protective signal of impending tissue damage that arises from stepping on a tack, for example. Inflammatory pain results from the activity of immune cells, as in osteoarthritis. And neuropathic pain springs from nerve damage that results from diabetes or chemotherapy, for instance. Fibromyalgia has been a conundrum in part because it doesn’t really fit into any of those categories, though some symptoms resemble inflammatory pain, and others neuropathic pain. Over the years, researchers have tried to craft a new category to contain Fibromyalgia, which they have variously called functional, dysfunctional, or somatoform disorders. “The term that we prefer is ‘centralized pain,’ meaning that pain clearly is coming largely from the brain rather than from out in the periphery,” says Rheumatologist Daniel Clauw, University of Michigan, Ann Arbor, US. Because the pain of Fibromyalgia seems to originate from the muscles, for years Rheumatologists studied patients’ muscle and joint tissues, but found no evidence of inflammation or damage that could cause pain. Without evidence for bodily injury underlying the pain, many researchers turned to studying the brains of people with Fibromyalgia. Some, including Clauw, have embraced the idea that Fibromyalgia is primarily a disease of the brain. The unifying symptoms, like widespread pain and fatigue, of Fibromyalgia and other such syndromes indicate that changes in the central nervous system are at play, Clauw says. Brain imaging studies have indeed shown evidence of structural and functional changes in the brains of patients with Fibromyalgia. And anti-depressant and anti-seizure medications that are effective for some people with Fibromyalgia work in the brain, he adds. But other researchers contend that all chronic pain conditions lead to changes in the brain, and in fact every experience of pain - whatever its initial cause - emerges from the brain. Many researchers in the field therefore are still searching for as-yet-undetected pathological processes in the body that may be driving the symptoms of Fibromyalgia - processes that might be reversible. Evidence of peripheral nerve damage In 2013, several groups published evidence of neuropathy, or damage and dysfunction, in the small nerve fibers that transmit pain signals from the skin, in patients diagnosed with fibromyalgia. One study led by Claudia Sommer, University of Würzburg, Germany, found dysfunctional nerve activity in twenty-five adults with fibromyalgia, according to sensory testing (in which subjects reported when they detected hot or cold stimuli) and electrical recordings of peripheral nerve activity. In addition, skin biopsies from Fibromyalgia patients often revealed withered or sparse nerve endings. These abnormalities were not present in healthy control subjects or in ten subjects without pain but with depression, a condition that shares some aspects of Fibromyalgia such as fatigue and inactivity. Another study, led by Anne Louise Oaklander at Massachusetts General Hospital, Boston, US (see related RELIEF podcast with Oaklander here) also used skin biopsies, with similar findings. Oaklander found that forty-one percent among 27 adult subjects meeting diagnostic criteria for Fibromyalgia also met the diagnostic criteria for small-fiber polyneuropathy (SFPN), a common neuropathic pain condition with myriad causes, whereas only 3% of healthy control subjects showed signs of SFPN. A third study, led by Jordi Serra, MC Mutual, Barcelona, Spain, and Neuroscience Technologies, London, UK, measured dysfunctional nerve activity in the peripheral nerves of fibromyalgia patients and showed that it mimicked nerve activity seen in patients with SFPN but not healthy controls. Serra uses a highly specialized technique called microneurography to record activity from individual nerves in a person’s skin. Together, these reports suggest that, somehow, damage to or dysfunction of peripheral nerves is a contributing factor in many cases of what has been diagnosed as Fibromyalgia. But many questions remain about the link between neuropathy and Fibromyalgia. Oaklander stresses that it’s important to identify any potential underlying medical causes of Fibromyalgia because some can be halted or improved. Most cases of SFPN can be traced to potentially treatable conditions including diabetes, chemotherapy for cancer, an autoimmune reaction, or rarely a genetic abnormality; some cases of SFPN remain mysterious in origin. Oaklander says that many of her patients with neuropathies have improved with treatment of these underlying conditions rather than relying on a standard course of treatment with painkillers. Certainly, not all cases of Fibromyalgia are rooted in undiagnosed SFPN, Oaklander says, “but pulling out the 40% who appear to have SFPN may help researchers to find the cause in the remaining 60% as well.” But for patients, a diagnosis or even treatment of SFPN may not be sufficient to halt Fibromyalgia. Kathleen Sluka, University of Iowa, Iowa City, US, says that while the findings of peripheral neuropathy in Fibromyalgia patients are an important piece of the puzzle, “patients need to understand this is not going to lead to a miracle cure. There are multiple mechanisms underlying Fibromyalgia, and there may be several going on at once. Treatments need to be aimed at each of those components and tailored to the individual,” she explained. Is it a real thing? While Fibromyalgia has gained recognition in recent years as a condition with biological underpinnings, many doctors practicing today still doubt that Fibromyalgia is real, or they refer to it as a psychological disorder - one that’s “all in the head.” But, like many diseases in the history of humankind, Serra says, Fibromyalgia is evolving in our cultural consciousness. For example, 200 years ago, people with epilepsy were regarded as crazy, or possessed by the devil. Only when electroencephalography (EEG) came along - a test that records brain activity using electrodes attached to the scalp - did doctors realize that the disease was rooted in abnormal brain activity. “Now, no one doubts that epilepsy is a neurological condition that can be treated. But back then, it was impossible to convince doctors it was a real disease. Fibromyalgia is very similar, in that we have patients who complain of pain and other mysterious symptoms and are studied by physicians who find nothing wrong,” so they often dismiss or ignore the patients, Serra says. That dismissal can make patients feel crazy, even though they know their pain is very real. “One of the most frustrating things for patients is that they are often not believed—and this may be constant, going on for years,” Serra says. While the new findings of peripheral nerve damage in fibromyalgia patients may not offer a cure or even an immediate treatment, they represent the first objective, physical evidence of dysfunction linked to their illness. “The skin biopsies and microneurography are objective tests. To have a doctor say your nerve activity is abnormal, or that you have small-fiber neuropathy” can be a source of tremendous relief and validation for patients, Serra says. It’s entirely possible that, until now, studies have missed signs of damage or dysfunction in nerves, Serra says, because they were undetectable with the relatively blunt diagnostic tests used in the past. Peripheral nerves, Serra says, are incredibly sensitive to slight changes in their surroundings, which can alter their activity. “The excitability of nerves is very fine-tuned,” he emphasizes. For example, a pain nerve fiber might be spontaneously active, but once the patient relaxes, that activity stops. That might happen because the patient’s breathing slows, perhaps changing the acidity of blood, or some other factor in the nerve fiber’s environment. “Just this little change in balance determines whether the nerve is firing or not firing,” Serra says. This finding, he explains, also fits with the relationship between stress and pain. “We know this—all patients say, ‘when I’m stressed, I’m worse, and when I’m relaxed, I feel better.’” Stress and trauma have long been known as contributing factors in Fibromyalgia, but researchers are still struggling to find out how they increase risk. “We know that psychology is strongly associated with chronic pain,” Staud says. “Emotional trauma is one of the vulnerabilities for the pain modulatory system, and families with emotional disorders are at much higher risk for chronic pain than others.” Genetic differences in genes associated with pain or stress, for example—may explain some of that risk, but traumatic experiences seem to accelerate the development of Fibromyalgia, even in the absence of physical injury. “Clearly any kind of stress or trauma can bring it on, whether it’s physical, emotional or even a stress on the immune system,” Clauw says. “That includes everything from early-life trauma to a major auto accident to the psychological stress of being deployed to war. Stress is so important.” Today, researchers are actively investigating what types of substances might circulate in the blood or affect the brain to link stress with Fibromyalgia. The top contenders include stress hormones and inflammatory molecules released by immune cells in the brain or body. End of the line? Many researchers agree that what is now called Fibromyalgia—characterized by widespread pain, fatigue, and cognitive and emotional disturbances—may be the final station on the chronic pain track. “Fibromyalgia is the endpoint—the end of the continuum,” says Clauw. “And maybe we can prevent people from getting there if we identify their risk early and treat aggressively,” which might include anti-depressant medications shown to improve Fibromyalgia pain in some patients, he says. Staud went further, saying that everyone might be at risk for chronic pain. “It’s not just the end of the line for chronic pain patients; it’s the end of the line for all of us.” How quickly we get there, he says, depends on how well we can fend off risks. “If you avoid significant trauma in life, be it physical or emotional, that can help keep your pain modulatory system very active and competent.” Otherwise, he says, “you get closer to chronic pain.” Of course not everyone develops chronic pain; some people seem to be protected for life. “For some, it’s a very flat trajectory toward that endpoint; for others, it’s very steep.” How can people build up this protection to stave off chronic pain? Staud says there are four concrete steps to take in order to minimize risk, whether an individual already has chronic pain or not. First, prevention of injuries or other traumatic events that can lead to pain is important. Of course, this is not always possible, but for someone with Fibromyalgia, it might mean avoiding stressful situations that could trigger a pain episode. Second, Staud says, physical exercise seems to condition the body against pain. Third, sleep is also protective, so getting as much high-quality sleep as possible will help. Finally, psychological coping skills are protective against pain. “The ability to adapt to stress of all sorts is critical,” Staud says. Cognitive-behavioral therapy (CBT), mindfulness, and supportive social interactions can all help build this resilience. However, Staud says, “there is a relatively small group of people who practice these steps consistently and effectively. The majority of the population does not.” Staud stresses that all of these recommendations require tremendous effort on the part of the patient—effort they might not be able to expend. Telling people with fibromyalgia to exercise, sleep more and get therapy, he says, “is similar to telling poor people to save more money and be frugal in order to get rich.” Staud says the emphasis in pain care should instead be on prevention and early recognition, and then on building financial, social and emotional support for patients. But, for those who are able to exercise, Sluka says the research shows that physical activity is perhaps the single most effective approach to alleviate chronic pain. “In the scientific literature, there is strong support for exercise as a way to mitigate pain—it’s one of the most effective treatments,” but only recently are doctors coming around to the idea of “prescribing” exercise for pain. Inactivity, she says, which is common in Fibromyalgia patients, might contribute to or even cause some symptoms of Fibromyalgia. “Research shows that higher physical activity leads to greater pain inhibition, it can improve cutaneous nerve innervation [the health and number of nerve fibers supplying the skin], and it can alter the immune system. Exercise does wonderful things.” Sluka also says it is important that patients play an active role in setting the course for their treatment, though this does place an additional encumbrance on patients already bearing the burden of chronic pain. “Patients need to take control and help manage their own condition,” Sluka says. That’s for two reasons: first, because things like improving sleep and getting exercise, which are under a patient’s control, may lessen pain and improve function. And second, by gaining a sense of control, patients can reduce their stress and pain. Finding a doctor who recognizes fibromyalgia and is willing to try different approaches is also crucial. Some people suffer from Fibromyalgia for years, seeing only doctors who tell them there’s nothing wrong with them, or they undergo surgery that doesn’t help, and they become discouraged. “For a lot of people, this is a long struggle. They end up beaten down, feeling helpless and hopeless,” Clauw says. When Clauw encounters these patients, he says it’s very difficult to help them. “We have to attempt to prop them up and reinvigorate them. Patients have to embrace the fact that there are things they have to do to get better. We can’t give them a drug to cure this - we can’t do that with any pain condition. The goal is to get pain appropriately diagnosed and treated early on, so they don’t get to that end of the pathway.” “The notion that there’s nothing we can do for people with Fibromyalgia is really just wrong,” Clauw says. “When you look at everything available, there is almost always something that will help.” It’s important to try different medications and nondrug therapies, he says, because which treatments may work will vary from person to person. Although many questions about the causes and treatment of Fibromyalgia remain unanswered, Serra says, “it’s a very exciting moment in pain research. We’re beginning to see things we couldn’t even imagine. We will begin to make sense of this disease soon.” Stephani Sutherland, PhD, is a neuroscientist, yogi, and freelance journalist in Southern California. Find her at StephaniSutherland.com or on Twitter @SutherlandPhD Additional Reading:
Related RELIEF content:
By Stephani Sutherland Your comment will be posted after it is approved.
Leave a Reply. |
Physioplus+Appearing here will be articles, information, case studies news and tips. Archives
July 2024
Categories |

 RSS Feed
RSS Feed
11/10/2019
0 Comments