 Initial assessment is done using the Montreal Cognitive Assessment Test to give us a baseline of how your memory is doing at the moment. Please let us know if you are dyslexic beforehand, as it can affect the results and may also mean the test needs to be adapted a bit. There isn't a lot of reading. Then the fun bits start ! As with most of our treatments, you will lie down on our comfy couch and we will gently assess the cause of your symptoms. It usually boils down to a decrease in circulation and/or flow of cerebrospinal fluid (CSF) around the brain, basically, the feeding and cleaning up team that keeps your brain cells healthy. In early stage memory loss, there is sometimes an area of gliosis (minor cell damage) around the outside of one of the lobes of the brain. We use techniques taught by Ted Wanveer MD (see references) to gently move brain structures and promote healing. At the same time, we go on a detective journey to see what is causing the decrease in nutrient flow and waste removal. The usual culprits are the foramina (holes that are supposed to be there!) in the temporal bone at the base of the skull. Problems elsewhere in your body can alter their position or angle and restrict fluid flow. Most commonly the problem is in the neck, but we have found altered foot position, previous back or disc problems and other unexpected areas contributing to the issue. Depending on where the problem originates, we will give exercises to solve the cause if possible, and probably a set of tennis balls to use at the base of your skull to gently stretch the soft tissue and give more space for the temporal holes and the structures that pass through them. We will retest you every 4 to 6 weeks. Based on our experience so far, we recommend treatment once/twice per week for 4 weeks, slowly tailing off as improvements occur. Expect a course of between 12 and 16 sessions. Unfortunately, once there is already a diagnosis of Alzheimer's Disease or Vascular Dementia, it is too late for treatment to be started, as we have found that although it MAY slow progress, it certainly doesn't stop the disease process from developing and we are unwilling to start treatment or give false hope knowing this. If this sounds like you or someone close please call 01287 201006 on a weekday morning 9 am to 12 midday to make an appointment. a few thoughts on ... not just a physio
We have your best interests at heart. One of the most important stages is to understand the current problem but perhaps more importantly the cause and at the same time your medical and health history. Physioplus+ has 2 parts of a successful treatment
Ultimately, solve the causes not just the symptoms ... and as a practice we always moderate our promises and then work towards over-delivering So to understand and investigate what can do, look at, treat and solve - click on Specialisms below PhysioPlus+ - Specialisms To get your treatment started telephone 01287 201006 Mon to Fri between 9 am and 12 noon oh ... and tell your friends ... all of them Craniosacral Therapy assists the body's natural ability to heal using gentle manual techniques, offering relief from pain and stress. This therapy is suitable for a wide range of pain symptoms.
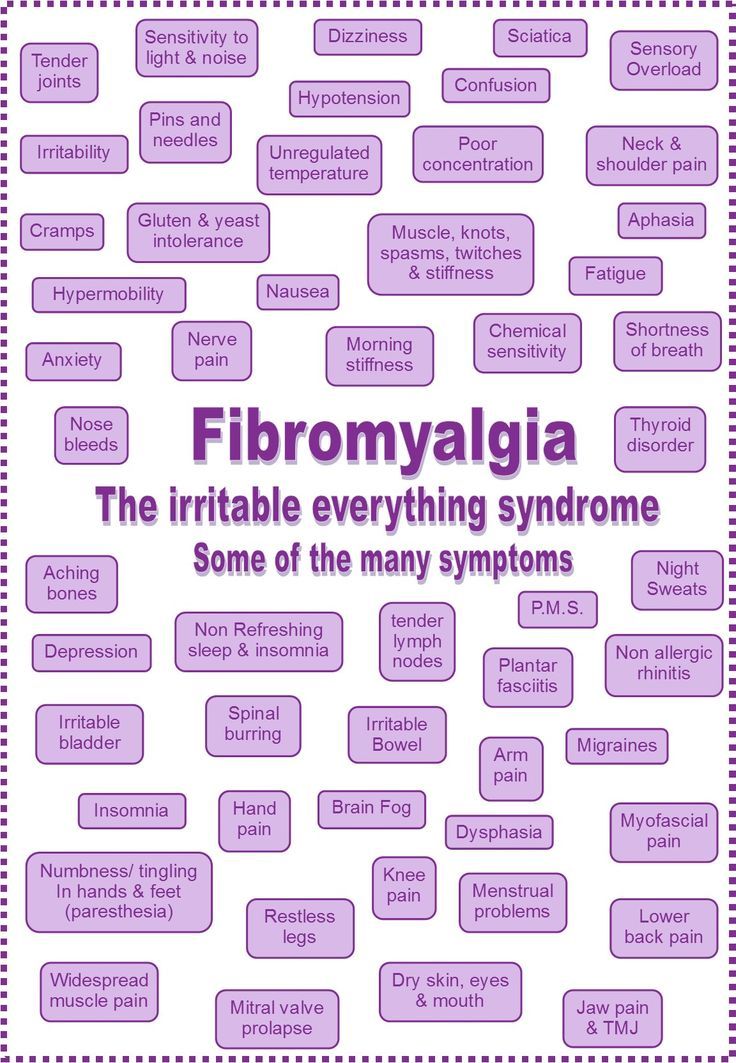
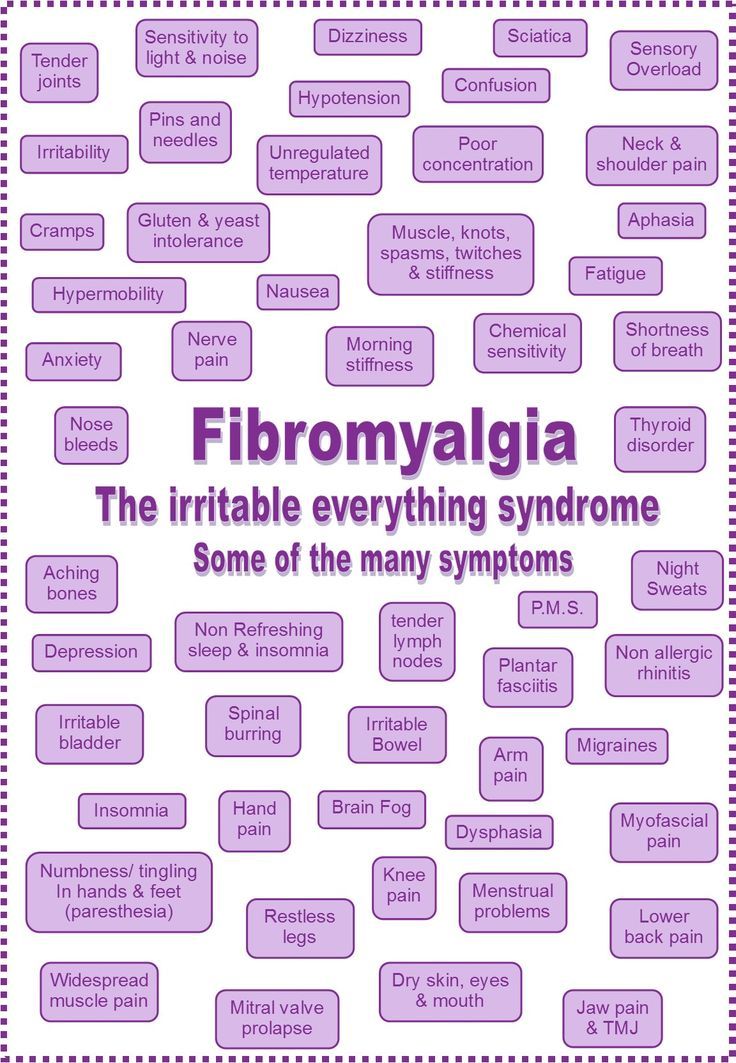
Craniosacral Therapy is a respectful treatment which improves overall wellbeing. We all have things happen to us in life that can cause dysfunction in our bodies. A trip up a step, a sporting injury or a car accident. Our bodies compensate for this but may develop tension patterns which cause symptoms from stiffness to pain. This is also the case with emotional stresses, causing headache, neck stiffness and a whole range of other symptoms from tiredness to anxiety. Craniosacral Therapy helps bring the body back into balance so you can get on and live your life fully. We need to listen to our bodies as they know what changes are necessary to keep them healthy. Our bodies speak to us most of the time, but we aren't very good at listening to them. Eventually we pay the price. Sometimes our assumptions about ourselves and our lives cause strain on the body. Craniosacral Therapy and Somato Emotional Release help identify these assumptions using incisive questions to free them. Touch with quality attention creates an environment for communication between the mind and body to facilitate healing. When therapists at Physioplus+ are undertaking Patient Treatment we will take a full case history, listening with care, to allow the creation of a plan of treatment specifically for the patient. During treatment, the patient will lie fully clothed on a treatment couch, or if this is not comfy on their side or sitting. The therapist places her hands gently on the patient's body to locate areas of reduced tissue motion and uses manual techniques to release these areas. Patients may notice a change immediately or gradually. Most people find the treatment relaxing. Afterwards patients may feel energised, tired, or no different to normal. It's a very individual thing. Sometimes during a treatment memories surrounding a past injury or shock may be recalled. This is Somato-Emotional Release. It helps patients to reconnect with what they are feeling in their body and return to optimal health. Therapists will work with the patient using visualisation and dialogue to explore what is coming up in a respectful way. When stressed, we become tense and trapped in our thoughts and anxieties which causes pain and discomfort. Working in this client-centered way is very effective in facilitating personal growth and promoting wellbeing. Contact for treatment by telephone - Physioplus+ on 01287 201006 We will be starting a pain-free exercise class for those with Fibromyalgia when we have sufficient interested patients.
The general opinion now seems to be that there is some sort of central nervous system irritation that leads to the widespread symptoms of Fibromyalgia. Raised levels of inflammation have been found in the central nervous system of Fibromyalgia patients, but is this a symptom or the cause? Still to be discovered. The symptoms remain difficult to manage We will be doing very gentle neurological stretches in the classes, and some body-centred relaxation and mindfulness techniques for pain and relaxation. Each participant will have a brief assessment of their personal nerve structure at the first session so that exercises can be tailored individually. The class will run initially for 10 weeks, and for longer if enough participants wish to continue. Classes will take place at Physioplus+, 25-27 Redcar Road, Guisborough, TS14 6HR. The first session will be assessment, a cup of tea or coffee and cake, and essential form filling with assistance to show your pain patterns and comply with data protection regulations. Follow-up sessions will be gentle individual exercise and group relaxation. Please bring a pillow or two so that you can lie comfortably on the floor or sit comfortably in a chair for this. Booking is essential, as numbers will be limited to ten participants. You need to ring 01287 201006 between 9:00am and 12:00 noon to book with Christine, our practice manager stating that you want to join the fibromyalgia class. If you sleep in the mornings, leave a message on the answerphone with your number, and mention the Fibromyalgia class and best time to ring so that we can get back to you. If the class fills quickly we will have a waiting list, or possibly put on an evening class at a later date. Payment is required in advance by credit or debit card, cheque or cash. You will only pay for EIGHT classes, as it is expected that you may miss a couple due to brain fog or a bad day. Each class will be run by a physiotherapist with many years of experience in Fibromyalgia assessment and treatment. Please also read this excellent article (below) by Stephani Sutherland on current research. https://www.physioplusguisborough.co.uk/articles/relief-pain-research-news-insights-ideas-by-stephani-sutherland Pain-free Fibromyalgia Classes in Guisborough at Physioplus+ https://www.physioplusguisborough.co.uk/articles/pain-free-fibromyalgia-classes-in-guisborough
Fibromyalgia: Cracking the Case Researchers are just beginning to understand the biological underpinnings of a long-misunderstood condition. Fibromyalgia. Many patients with this perplexing diagnosis have seen doctor after doctor in search of an explanation for the widespread pain, fatigue, and disordered sleep that has disrupted their lives - sometimes severely. Depression, anxiety, and “brain fog” also commonly affect people with Fibromyalgia. Despite decades of research, seemingly everything about Fibromyalgia remains mysterious. But, encouragingly, researchers are finally making progress toward understanding this long-unexplained syndrome. Those who study Fibromyalgia hope this will legitimize a condition that physicians have long doubted, and bring much-needed relief to patients. A difficult diagnosis Not everyone with all-over pain receives the diagnosis of Fibromyalgia. The label usually comes from a Rheumatologist - a doctor who specializes in musculoskeletal and autoimmune disorders - only after other ailments are ruled out. But other chronic pain diagnoses, including temporomandibular joint disorder (TMJD), chronic pelvic pain conditions such as interstitial cystitis (IC), and irritable bowel syndrome (IBS) often mimic the symptoms of Fibromyalgia, also often with no discernible physical cause. The diagnosis that a patient receives might depend on the specialist they see, experts say. Roland Staud, University of Florida, Gainesville, US, likens the current understanding of fibromyalgia to the traditional Indian story of seven blind mice trying to determine the identity of an elephant. One blind mouse feels a leg and calls it a pillar; another grabs ahold of the tail and reports finding a rope. Not until all the parts are considered as a whole does a complete picture of the beast emerge. Likewise, Rheumatologists with patients complaining of muscle aches may diagnose Fibromyalgia, whereas a gastroenterologist proclaims IBS the cause of pain, but apart from complaints of regional pain in IBS, the overall symptoms of these two conditions look remarkably similar. Patients with low back pain, osteoarthritis, and other common chronic pain conditions can also develop this characteristic set of symptoms. Today, researchers are sketching out a picture of Fibromyalgia as a pain disorder that can be triggered by any number of individual maladies, each one heightening future risk for developing this enigmatic condition. Brain pain? Researchers and doctors have traditionally classified different types of pain into several categories. Nociceptive pain is the acute protective signal of impending tissue damage that arises from stepping on a tack, for example. Inflammatory pain results from the activity of immune cells, as in osteoarthritis. And neuropathic pain springs from nerve damage that results from diabetes or chemotherapy, for instance. Fibromyalgia has been a conundrum in part because it doesn’t really fit into any of those categories, though some symptoms resemble inflammatory pain, and others neuropathic pain. Over the years, researchers have tried to craft a new category to contain Fibromyalgia, which they have variously called functional, dysfunctional, or somatoform disorders. “The term that we prefer is ‘centralized pain,’ meaning that pain clearly is coming largely from the brain rather than from out in the periphery,” says Rheumatologist Daniel Clauw, University of Michigan, Ann Arbor, US. Because the pain of Fibromyalgia seems to originate from the muscles, for years Rheumatologists studied patients’ muscle and joint tissues, but found no evidence of inflammation or damage that could cause pain. Without evidence for bodily injury underlying the pain, many researchers turned to studying the brains of people with Fibromyalgia. Some, including Clauw, have embraced the idea that Fibromyalgia is primarily a disease of the brain. The unifying symptoms, like widespread pain and fatigue, of Fibromyalgia and other such syndromes indicate that changes in the central nervous system are at play, Clauw says. Brain imaging studies have indeed shown evidence of structural and functional changes in the brains of patients with Fibromyalgia. And anti-depressant and anti-seizure medications that are effective for some people with Fibromyalgia work in the brain, he adds. But other researchers contend that all chronic pain conditions lead to changes in the brain, and in fact every experience of pain - whatever its initial cause - emerges from the brain. Many researchers in the field therefore are still searching for as-yet-undetected pathological processes in the body that may be driving the symptoms of Fibromyalgia - processes that might be reversible. Evidence of peripheral nerve damage In 2013, several groups published evidence of neuropathy, or damage and dysfunction, in the small nerve fibers that transmit pain signals from the skin, in patients diagnosed with fibromyalgia. One study led by Claudia Sommer, University of Würzburg, Germany, found dysfunctional nerve activity in twenty-five adults with fibromyalgia, according to sensory testing (in which subjects reported when they detected hot or cold stimuli) and electrical recordings of peripheral nerve activity. In addition, skin biopsies from Fibromyalgia patients often revealed withered or sparse nerve endings. These abnormalities were not present in healthy control subjects or in ten subjects without pain but with depression, a condition that shares some aspects of Fibromyalgia such as fatigue and inactivity. Another study, led by Anne Louise Oaklander at Massachusetts General Hospital, Boston, US (see related RELIEF podcast with Oaklander here) also used skin biopsies, with similar findings. Oaklander found that forty-one percent among 27 adult subjects meeting diagnostic criteria for Fibromyalgia also met the diagnostic criteria for small-fiber polyneuropathy (SFPN), a common neuropathic pain condition with myriad causes, whereas only 3% of healthy control subjects showed signs of SFPN. A third study, led by Jordi Serra, MC Mutual, Barcelona, Spain, and Neuroscience Technologies, London, UK, measured dysfunctional nerve activity in the peripheral nerves of fibromyalgia patients and showed that it mimicked nerve activity seen in patients with SFPN but not healthy controls. Serra uses a highly specialized technique called microneurography to record activity from individual nerves in a person’s skin. Together, these reports suggest that, somehow, damage to or dysfunction of peripheral nerves is a contributing factor in many cases of what has been diagnosed as Fibromyalgia. But many questions remain about the link between neuropathy and Fibromyalgia. Oaklander stresses that it’s important to identify any potential underlying medical causes of Fibromyalgia because some can be halted or improved. Most cases of SFPN can be traced to potentially treatable conditions including diabetes, chemotherapy for cancer, an autoimmune reaction, or rarely a genetic abnormality; some cases of SFPN remain mysterious in origin. Oaklander says that many of her patients with neuropathies have improved with treatment of these underlying conditions rather than relying on a standard course of treatment with painkillers. Certainly, not all cases of Fibromyalgia are rooted in undiagnosed SFPN, Oaklander says, “but pulling out the 40% who appear to have SFPN may help researchers to find the cause in the remaining 60% as well.” But for patients, a diagnosis or even treatment of SFPN may not be sufficient to halt Fibromyalgia. Kathleen Sluka, University of Iowa, Iowa City, US, says that while the findings of peripheral neuropathy in Fibromyalgia patients are an important piece of the puzzle, “patients need to understand this is not going to lead to a miracle cure. There are multiple mechanisms underlying Fibromyalgia, and there may be several going on at once. Treatments need to be aimed at each of those components and tailored to the individual,” she explained. Is it a real thing? While Fibromyalgia has gained recognition in recent years as a condition with biological underpinnings, many doctors practicing today still doubt that Fibromyalgia is real, or they refer to it as a psychological disorder - one that’s “all in the head.” But, like many diseases in the history of humankind, Serra says, Fibromyalgia is evolving in our cultural consciousness. For example, 200 years ago, people with epilepsy were regarded as crazy, or possessed by the devil. Only when electroencephalography (EEG) came along - a test that records brain activity using electrodes attached to the scalp - did doctors realize that the disease was rooted in abnormal brain activity. “Now, no one doubts that epilepsy is a neurological condition that can be treated. But back then, it was impossible to convince doctors it was a real disease. Fibromyalgia is very similar, in that we have patients who complain of pain and other mysterious symptoms and are studied by physicians who find nothing wrong,” so they often dismiss or ignore the patients, Serra says. That dismissal can make patients feel crazy, even though they know their pain is very real. “One of the most frustrating things for patients is that they are often not believed—and this may be constant, going on for years,” Serra says. While the new findings of peripheral nerve damage in fibromyalgia patients may not offer a cure or even an immediate treatment, they represent the first objective, physical evidence of dysfunction linked to their illness. “The skin biopsies and microneurography are objective tests. To have a doctor say your nerve activity is abnormal, or that you have small-fiber neuropathy” can be a source of tremendous relief and validation for patients, Serra says. It’s entirely possible that, until now, studies have missed signs of damage or dysfunction in nerves, Serra says, because they were undetectable with the relatively blunt diagnostic tests used in the past. Peripheral nerves, Serra says, are incredibly sensitive to slight changes in their surroundings, which can alter their activity. “The excitability of nerves is very fine-tuned,” he emphasizes. For example, a pain nerve fiber might be spontaneously active, but once the patient relaxes, that activity stops. That might happen because the patient’s breathing slows, perhaps changing the acidity of blood, or some other factor in the nerve fiber’s environment. “Just this little change in balance determines whether the nerve is firing or not firing,” Serra says. This finding, he explains, also fits with the relationship between stress and pain. “We know this—all patients say, ‘when I’m stressed, I’m worse, and when I’m relaxed, I feel better.’” Stress and trauma have long been known as contributing factors in Fibromyalgia, but researchers are still struggling to find out how they increase risk. “We know that psychology is strongly associated with chronic pain,” Staud says. “Emotional trauma is one of the vulnerabilities for the pain modulatory system, and families with emotional disorders are at much higher risk for chronic pain than others.” Genetic differences in genes associated with pain or stress, for example—may explain some of that risk, but traumatic experiences seem to accelerate the development of Fibromyalgia, even in the absence of physical injury. “Clearly any kind of stress or trauma can bring it on, whether it’s physical, emotional or even a stress on the immune system,” Clauw says. “That includes everything from early-life trauma to a major auto accident to the psychological stress of being deployed to war. Stress is so important.” Today, researchers are actively investigating what types of substances might circulate in the blood or affect the brain to link stress with Fibromyalgia. The top contenders include stress hormones and inflammatory molecules released by immune cells in the brain or body. End of the line? Many researchers agree that what is now called Fibromyalgia—characterized by widespread pain, fatigue, and cognitive and emotional disturbances—may be the final station on the chronic pain track. “Fibromyalgia is the endpoint—the end of the continuum,” says Clauw. “And maybe we can prevent people from getting there if we identify their risk early and treat aggressively,” which might include anti-depressant medications shown to improve Fibromyalgia pain in some patients, he says. Staud went further, saying that everyone might be at risk for chronic pain. “It’s not just the end of the line for chronic pain patients; it’s the end of the line for all of us.” How quickly we get there, he says, depends on how well we can fend off risks. “If you avoid significant trauma in life, be it physical or emotional, that can help keep your pain modulatory system very active and competent.” Otherwise, he says, “you get closer to chronic pain.” Of course not everyone develops chronic pain; some people seem to be protected for life. “For some, it’s a very flat trajectory toward that endpoint; for others, it’s very steep.” How can people build up this protection to stave off chronic pain? Staud says there are four concrete steps to take in order to minimize risk, whether an individual already has chronic pain or not. First, prevention of injuries or other traumatic events that can lead to pain is important. Of course, this is not always possible, but for someone with Fibromyalgia, it might mean avoiding stressful situations that could trigger a pain episode. Second, Staud says, physical exercise seems to condition the body against pain. Third, sleep is also protective, so getting as much high-quality sleep as possible will help. Finally, psychological coping skills are protective against pain. “The ability to adapt to stress of all sorts is critical,” Staud says. Cognitive-behavioral therapy (CBT), mindfulness, and supportive social interactions can all help build this resilience. However, Staud says, “there is a relatively small group of people who practice these steps consistently and effectively. The majority of the population does not.” Staud stresses that all of these recommendations require tremendous effort on the part of the patient—effort they might not be able to expend. Telling people with fibromyalgia to exercise, sleep more and get therapy, he says, “is similar to telling poor people to save more money and be frugal in order to get rich.” Staud says the emphasis in pain care should instead be on prevention and early recognition, and then on building financial, social and emotional support for patients. But, for those who are able to exercise, Sluka says the research shows that physical activity is perhaps the single most effective approach to alleviate chronic pain. “In the scientific literature, there is strong support for exercise as a way to mitigate pain—it’s one of the most effective treatments,” but only recently are doctors coming around to the idea of “prescribing” exercise for pain. Inactivity, she says, which is common in Fibromyalgia patients, might contribute to or even cause some symptoms of Fibromyalgia. “Research shows that higher physical activity leads to greater pain inhibition, it can improve cutaneous nerve innervation [the health and number of nerve fibers supplying the skin], and it can alter the immune system. Exercise does wonderful things.” Sluka also says it is important that patients play an active role in setting the course for their treatment, though this does place an additional encumbrance on patients already bearing the burden of chronic pain. “Patients need to take control and help manage their own condition,” Sluka says. That’s for two reasons: first, because things like improving sleep and getting exercise, which are under a patient’s control, may lessen pain and improve function. And second, by gaining a sense of control, patients can reduce their stress and pain. Finding a doctor who recognizes fibromyalgia and is willing to try different approaches is also crucial. Some people suffer from Fibromyalgia for years, seeing only doctors who tell them there’s nothing wrong with them, or they undergo surgery that doesn’t help, and they become discouraged. “For a lot of people, this is a long struggle. They end up beaten down, feeling helpless and hopeless,” Clauw says. When Clauw encounters these patients, he says it’s very difficult to help them. “We have to attempt to prop them up and reinvigorate them. Patients have to embrace the fact that there are things they have to do to get better. We can’t give them a drug to cure this - we can’t do that with any pain condition. The goal is to get pain appropriately diagnosed and treated early on, so they don’t get to that end of the pathway.” “The notion that there’s nothing we can do for people with Fibromyalgia is really just wrong,” Clauw says. “When you look at everything available, there is almost always something that will help.” It’s important to try different medications and nondrug therapies, he says, because which treatments may work will vary from person to person. Although many questions about the causes and treatment of Fibromyalgia remain unanswered, Serra says, “it’s a very exciting moment in pain research. We’re beginning to see things we couldn’t even imagine. We will begin to make sense of this disease soon.” Stephani Sutherland, PhD, is a neuroscientist, yogi, and freelance journalist in Southern California. Find her at StephaniSutherland.com or on Twitter @SutherlandPhD Additional Reading:
Related RELIEF content:
By Stephani Sutherland 17/9/2019 Frozen Shoulder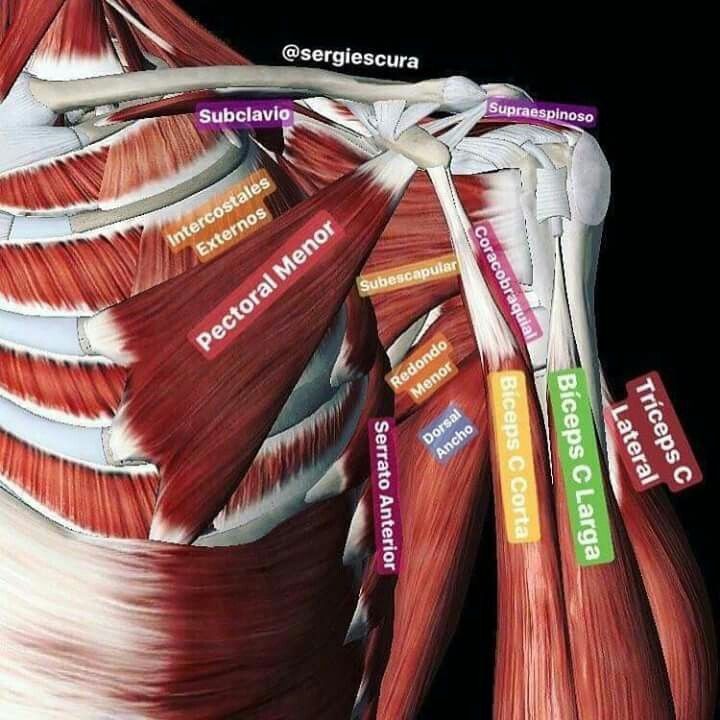 Do you have a "frozen" shoulder? The medical name for this condition is "adhesive capsulitis". In a true "frozen shoulder", movements are limited and painful in all directions because the capsule (which is the fibrous tissue that holds the shoulder together whilst allowing it to move) gets inflamed and painful, and involves other things around the shoulder, like nerves and connective tissue. It often gets confused with a rotator cuff injury, where just the shoulder muscle tendons get inflamed. Treatment is different for the two conditions. GP treatment options include:
We have found with experience over more than 30 years that the traditional physio approach of exercise and capsule manipulation is just too painful for most people with a frozen shoulder. After trying different treatment and pain-killing approaches, we found that combining acupuncture with gentle mobilisation gets the fastest results. The acupuncture controls the pain whilst allowing movement to take place more easily. Typically, a course of this treatment combination takes about eight sessions to solve the problem to about 90% ( which we achieve with over 90% of our patients) and people can then work with exercises themselves to get the last bits of movement. It really doesn't matter how long you have had it for, although if you have been putting up with it for many years, it may take a little longer. Often people are told that if will "sort itself out" in about eighteen months, so they don't even think of trying to get help before then. Sooner works better! Think you have a frozen shoulder? Come and see our shoulder specialist who will check your diagnosis and then treat you! See our website at www.physioplusguisborough.co.uk for assessment and treatment prices, and case studies for shoulders and other conditions. Appointments can be made by telephone to our practice in Guisborough between 09:00 am and 12:00 noon, or by leaving your number on our answerphone outside those hours. We do daytime and evening appointments - 01287 201006 22/7/2019 Problem - Swollen Feet & AnklesWhat is causing my swollen feet and ankles?
Most likely: water retention. As we get older, healthy function in the autonomic nervous system and lymphatic system can decrease. The autonomic nervous system controls things like body temperature, blood pressure, blood circulation etc. The lymphatic system is responsible for clearing micro waste products, and is an essential part of the immune system. If either system isn’t working at optimum level, the blood vessels in your legs may allow excess fluid (water, lymph) to “pool” in your legs and sometimes in your hands, especially in hot weather, or after prolonged sitting. It is common to get swollen ankles after a plane journey too, due to the combination of sitting and altered pressure in the aeroplane. But if they stay swollen, it is often the autonomic nervous system or the lymphatic system to blame. Symptoms Swollen, usually painless ankles and feet, with shoes feeling tighter, and/or swollen, usually painless fingers and your rings feel too tight. In hot weather, alteration in salt levels in your system due to sweating makes the problem worse. Self-help: wear flight socks for flights and move around the plane. Sit with your feet up whenever possible. “Paddle” your feet up and down whenever you are sitting to help the leg muscles to push the fluid up your legs. Flap your hands up and down if your fingers are affected, or regularly grip and release your hands, sit with your hands above your head for a while to let gravity help! If the weather is hot, drink more fluids, as this stops salt concentration. Decrease alcohol and caffeine consumption as they dehydrate you. Your GP may be able to prescribe a mild water tablet such as bendroflumethiazide for use just before flights, or during your holidays to hot climates. This obviously depends on what other medication you are using. Treatment If this is happening very regularly, and the exercises haven’t helped, lymphatic drainage massage or acupressure massage can help – call us to make an appointment. GP Visit Required More serious causes: heart and kidney disease can lead to swollen feet and ankles, so get a check up from your GP. Immediate Medical Attention If only one leg swells, especially if it is also tender when you squeeze your calf or it is hot when you touch it, you should seek IMMEDIATE medical attention, this can be a sign of DVT (deep vein thrombosis), a blood clot in the leg that can lead to stroke or pulmonary embolism (blood clot on the lung), both of which can be fatal. 22/7/2019 Case History - Frozen Shoulder “Frozen” shoulder is used to describe a range of problems which occur around the shoulder joint, which ultimately result in restriction of movement and pain on movement of the shoulder. In its truest form, “frozen” shoulder refers to a condition called adhesive capsulitis in medical terminology. The shoulder capsule is a structure which is designed to hold the parts of the shoulder joint together securely and allow for lubrication to be supplied to the joint. In adhesive capsulitis this structure becomes restricted due to inflammation and pain, and can take a long time to resolve on its own. Patient Mrs A Mrs A a 66-year-old in good health, came to see our shoulder specialist, for treatment to her shoulder. She had had right shoulder pain for 2 years, and it was gradually worsening. Her range of movement had decreased to about 50% of normal, she couldn’t sleep on her right side due to the pain, and pain killers weren’t helping. She had had a few sessions of sports massage at another clinic, which hadn’t helped. Assessment Stage We assessed her and diagnosed adhesive capsulitis and explained the diagnosis and treatment options to Mrs A. Treatment Stage Treatment started with acupuncture for pain relief, along with gentle joint mobilisation and home exercises to gradually restore movement. By her 8th treatment (once weekly for eight weeks), she had full pain-free movement again. Please contact Physioplus+ Reception to make an Appointment to be Assessed should you be experiencing any kind of similar pain or symptoms - 01287 201006 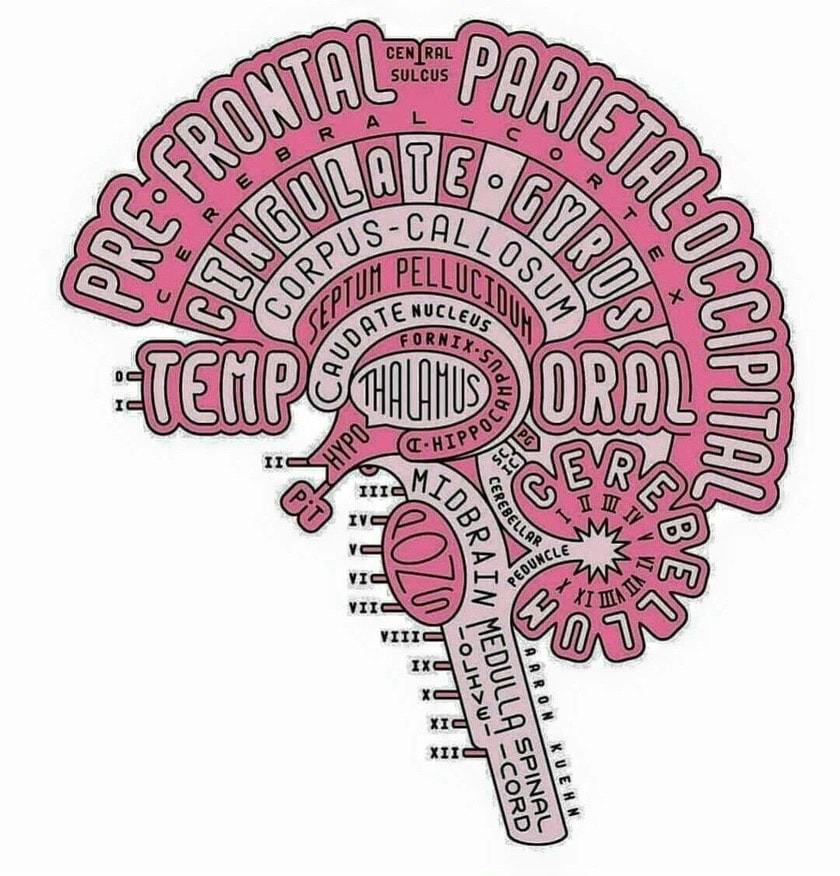 Here is the Link to a great post on LinkedIn starting with a post from Neuroscience News LinkedIn Article Widespread Inflammation in Brains of Those with Fibromyalgia Researchers documented widespread inflammation in the brains of patients with the poorly understood condition called fibromyalgia. The research is in Brain, Behavior and Immunity. (full open access) hashtag#inflammation hashtag#research hashtag#fibromyalgia hashtag#neurology hashtag#health hashtag#science hashtag#medicine hashtag#neuroscience Here is Jane's response This supports the theory that fibromyalgia is caused by irritation/inflammation in the nervous system, causing pain in the peripheral nerves, and the typical "brain fog" and fatigue that sufferers report. Both can be effectively treated by doing very gentle, pain free nerve stretches, and by use of cranio-sacral therapy to improve fluid flow around the nervous system to remove inflammation. High potency CBD oil also helps, as it targets cannabidiol receptors without the side effects common to e.g. gabapentin or high strength painkillers, which tend to add to fatigue and brain fog symptoms. hashtag#health hashtag#research hashtag#pain hashtag#inflammation hashtag#cbd hashtag#fibromyalgia hashtag#chronicpain  Failed with pelvic floor exercises and electrical devices? Incontinence still a problem? Got a prolapse as well? Come and get it fixed. We use a unique combination of cranio-sacral therapy combined with nerve stretches to fix the problem. Everything in your body works because a signal goes down the nerves from you brain or spinal cord and tells it to. If your womb drops, or your pelvic floor stops working properly to hold everything up, or if you bladder (or bowel) starts leaking, or emptying when it shouldn't, it is because the nerves have stopped sending messages properly. Treatment is done fully clothed, by working on the connective tissue (which connects everything in the body together), usually from your head and your feet. It's a bit like pulling a piece of elastic and looking for any "knots" that may be stopping it from stretching properly. Sometimes we need to put a hand under the bottom of your back as well to do a little more stretching, still fully clothed. Once the nerves are mobile, they automatically make the muscles work again, so no exercises are needed. It isn't magic. It doesn't hurt. It fixes the problem. Don't take our word for it. This is what some of our patients have said: 'I went from wetting myself every time I bent down or laughed to star jumps in 3 sessions after having problems following the birth of my second child' KC I didn't know that this could be fixed by a physiotherapist. I only mentioned that I was having problems with bowel leakage because I was going for a hospital appointment. I can now go out without worrying at all or taking an extra set of clothes. The embarrassment has gone. Mrs M |
Physioplus+Appearing here will be articles, information, case studies news and tips. Archives
July 2024
Categories |

 RSS Feed
RSS Feed
2/7/2024
0 Comments